At a time of the growing epidemic of opioid addiction and overdose, this study delivers an important message to general practitioners and healthcare professionals in primary care centers or nursing homes: the clinical importance of continuity of the doctor-patient relationship in the prescription of opioids. This team from the University of Oregon shows in the Annals of Family Medicine, through the analysis of data from nearly 2 million patients, that patients who have benefited from the greatest continuity of opioid prescription have received fewer “risky prescriptions” and experienced fewer opioid-related hospitalizations.
The prescription of opioids has increased dramatically in recent years and with this increase comes an increase in overdoses, deaths and addiction treatments. In an effort to reduce these risks, clinical guidelines emphasize prescriber continuity for prescribing opioids. Little is known, however, about how prescriber continuity influences risky prescribing patterns or overdose risk.
The team sought to better understand the association between continuity of opioid prescribing, different risky prescribing patterns, and patients' risk of overdose. Using data from the Oregon Prescription Drug Surveillance Program, the researchers selected patients with prolonged opioid use. A continuity of care index was calculated for each patient, parameters characterizing the prescriptions and the risk of overdose were identified.
A complex but precise methodology: the researchers took into account the number of prescriptions for each patient, each category of drug and each 6-month period. To calculate the continuity of the prescription index, the researchers identified, for each patient, their prescriber then measured the continuity of care index: the index representing the total number of prescribers over periods of 6 months and more.of the prescriber identified as the main one. Patients with prolonged use of opioids were finally divided into quartiles according to this index and this classification was compared to the adverse effects identified related to opioids. At-risk opioid prescriptions were calculated for each patient during each of the 6-month periods: an inappropriate opioid prescription is a prescription written for the same opioid within 7 days of the prescription of at least 30 tablets from another prescriber. Opioid-related hospitalizations and deaths were identified using the International Classification of Diseases (ICD-9-CM and ICD-10-CM) diagnosis codes.
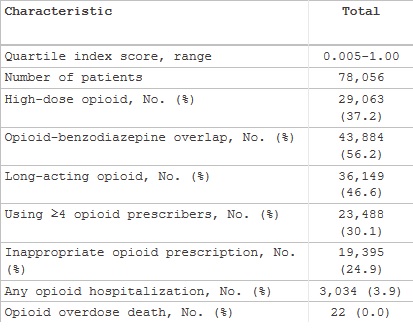
An epidemiology of opioid (and stimulant and benzodiazepine) use - see table below : during the study period,
- 1.7 million patients were prescribed opioids,
- 78,056 (4.6%): patients with prolonged opioid consumption;
- 119,529 (7%) who received a prescription for stimulants;
- 9,014 (7.5%) with long-term stimulant use.
- 596,978 patients received a prescription for a benzodiazepine and 31,437 (5.3%) were included as long-term patients.
Continuity data:
- Patients with greater opioid prescribing continuity received fewer risky prescriptions than patients in the lowest quartile,
- These patients are less likely to be hospitalized for opioid-related causes.
The analysis thus shows that more continuity in the prescription of opioids is associated with a reduction in the risk of hospitalization. Prescribing continuity is therefore an important marker of opioid harm.
The authors suggest that additional efforts may be needed to optimize this continuity.